Blog
Understanding Pressure Sores on the Lower Extremities
Pressure sores on the lower extremities develop when constant force on the skin reduces blood flow to the tissue. They often occur on the heels, ankles, and sides of the feet where bone is close to the surface. Limited mobility, wearing tight shoes, improper cushioning, and medical conditions that affect circulation can increase the risk. Early signs include redness, warmth, or tenderness that does not improve after pressure is relieved. More advanced sores may show blistering, open wounds, or deeper tissue damage. Treatment focuses on relieving pressure, protecting the skin, and supporting healthy blood flow. This may include padding the affected area, repositioning frequently, using supportive footwear, and applying appropriate wound dressings. Keeping the skin clean, moisturized, and monitored is important for preventing complications. Because pressure sores can progress quickly on the lower extremities, especially in people with diabetes or circulation issues, it is suggested that you see a wound care specialist if healing slows down, or symptoms worsen.
Pressure Sores, Pressure Ulcers, and Arterial Ulcers Can Lead to Skin Breakdown
Not all wounds on the feet, ankles, and legs are the same. Pressure sores, pressure ulcers, and arterial ulcers may look similar at first, but develop for different reasons and require specialized care. Understanding these differences is key to proper treatment.
Pressure sores are often caused by friction at common rubbing points. Toes rubbing against each other can create small raw areas, while wearing ill-fitting shoes may lead to sores on the heel, ankle, or sides of the foot. These injuries usually begin at the surface but can quickly deepen if ignored.
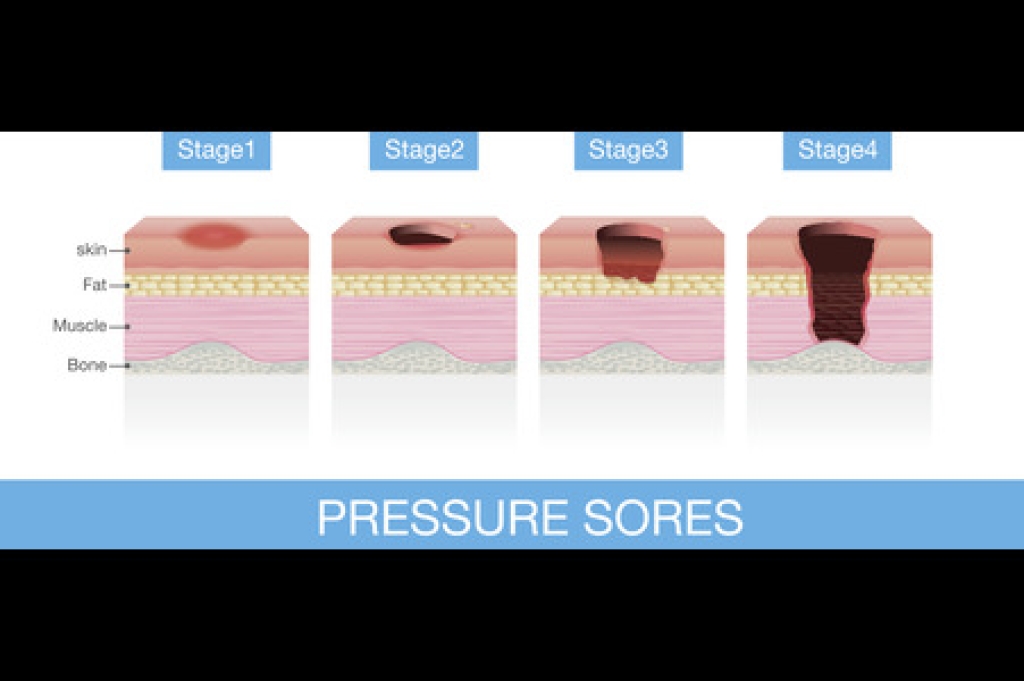
Pressure ulcers, sometimes called bedsores, occur when the skin and tissue are compressed between bone and an external surface for long periods of time. On the lower extremities, they frequently appear on the heels, ankles, calves, or shins. Limited mobility, tight footwear, or prolonged bed rest can all contribute to these ulcers, which may progress through multiple stages from redness to open, infected wounds.
Arterial ulcers are different in that they result from poor circulation. When blood flow to the feet and legs is reduced, oxygen and nutrients cannot reach the tissue. Even small sores on the toes, heels, or shins may become painful, deep ulcers that heal very slowly. Unlike friction-related sores, arterial ulcers are directly tied to vascular health and often signal an underlying circulation problem.
All three types of wounds demand professional attention. A wound care specialist can determine the cause, relieve pressure, improve circulation when possible, and use advanced techniques to promote healing.
If you notice a sore on your foot, ankle, or leg that is slow to close or worsening, call us for timely care to help prevent serious complications and preserve long-term mobility.
Recognizing Blistering Disorders of the Feet and Lower Legs

Blistering disorders are conditions where the skin becomes unusually fragile, leading to fluid-filled blisters that can appear even with minimal irritation. When these disorders affect the feet and lower legs, everyday friction from socks, shoes, braces, or swelling can make symptoms more noticeable. Autoimmune conditions such as bullous pemphigoid cause the body to attack its own skin, resulting in firm, often itchy blisters. Genetic conditions like epidermolysis bullosa create extremely delicate skin that blisters from light pressure or rubbing. Dermatitis herpetiformis, linked to gluten sensitivity, may show up as clusters of small, intensely itchy blisters on the lower limbs. Infections, medications, or allergic reactions can also trigger sudden blistering in these areas. Because these disorders can lead to slow healing, discomfort, and infection risk, it is suggested that you seek evaluation by a wound care specialist for an accurate diagnosis and appropriate care.
Why Blisters Can Be Risky for Leg and Foot Health
Blisters are small pockets of fluid that form beneath the skin, often as a result of friction, pressure, or burns. On the feet, ankles, and legs, they are particularly common because these areas endure daily stress from walking, running, and wearing shoes. While many blisters are minor, they can become serious if not treated correctly, especially in individuals with diabetes or poor circulation.
Friction is the most common cause of blisters. Shoes that are too tight, too loose, or not properly cushioned may rub against the heel, toes, or sides of the foot, leading to painful fluid-filled bubbles. Activities such as hiking, sports, or even long periods of standing can also trigger blisters, especially when combined with moisture from sweat.
Other blisters may form from burns, allergic reactions, or underlying medical conditions. On the lower extremities, blisters that break open expose the skin to bacteria, increasing the risk of infection and complicating the healing process. If a blister appears on the ankle, heel, or shin, it may interfere with walking and daily mobility.
Proper care begins with protecting the blister. Keeping the area clean, covered, and free from further friction supports healing. However, large, painful, or recurrent blisters often require professional evaluation. For patients with compromised circulation or nerve damage, even a small blister can turn into a much larger problem if ignored.
A wound care specialist can determine the cause, provide safe drainage if needed, and apply advanced dressings to promote recovery. They can also recommend changes in footwear, activity, or skin protection strategies to prevent future blisters.
If you have developed a blister on your foot, ankle, or leg that is not healing or is becoming more painful, make an appointment with us as soon as possible.
Restoring Circulation and Healing Arterial Leg Ulcers

Arterial ulcers occur when reduced blood flow prevents oxygen and nutrients from nourishing the skin, leading to slow-healing wounds on the legs, feet, or toes. These ulcers often develop in people with diabetes, peripheral artery disease, or poor circulation, and may appear small but feel painful. Wound care specialists provide targeted treatments designed to restore healing and comfort. This may include improving blood flow through vascular assessment, cleansing the wound, and applying advanced dressings that protect tissue and maintain moisture balance. Some patients benefit from compression therapy, gentle targeted exercises, or circulatory support to encourage faster recovery. Daily foot checks, smoking cessation, and proper hydration can also help prevent future ulcers. If you notice a sore on your leg or foot that is not healing, it is suggested that you schedule an appointment with a wound care specialist.
Pressure Sores, Pressure Ulcers, and Arterial Ulcers Can Lead to Skin Breakdown
Not all wounds on the feet, ankles, and legs are the same. Pressure sores, pressure ulcers, and arterial ulcers may look similar at first, but develop for different reasons and require specialized care. Understanding these differences is key to proper treatment.
Pressure sores are often caused by friction at common rubbing points. Toes rubbing against each other can create small raw areas, while wearing ill-fitting shoes may lead to sores on the heel, ankle, or sides of the foot. These injuries usually begin at the surface but can quickly deepen if ignored.
Pressure ulcers, sometimes called bedsores, occur when the skin and tissue are compressed between bone and an external surface for long periods of time. On the lower extremities, they frequently appear on the heels, ankles, calves, or shins. Limited mobility, tight footwear, or prolonged bed rest can all contribute to these ulcers, which may progress through multiple stages from redness to open, infected wounds.
Arterial ulcers are different in that they result from poor circulation. When blood flow to the feet and legs is reduced, oxygen and nutrients cannot reach the tissue. Even small sores on the toes, heels, or shins may become painful, deep ulcers that heal very slowly. Unlike friction-related sores, arterial ulcers are directly tied to vascular health and often signal an underlying circulation problem.
All three types of wounds demand professional attention. A wound care specialist can determine the cause, relieve pressure, improve circulation when possible, and use advanced techniques to promote healing.
If you notice a sore on your foot, ankle, or leg that is slow to close or worsening, call us for timely care to help prevent serious complications and preserve long-term mobility.


