Pressure sores on the lower extremities develop when constant force on the skin reduces blood flow to the tissue. They often occur on the heels, ankles, and sides of the feet where bone is close to the surface. Limited mobility, wearing tight shoes, improper cushioning, and medical conditions that affect circulation can increase the risk. Early signs include redness, warmth, or tenderness that does not improve after pressure is relieved. More advanced sores may show blistering, open wounds, or deeper tissue damage. Treatment focuses on relieving pressure, protecting the skin, and supporting healthy blood flow. This may include padding the affected area, repositioning frequently, using supportive footwear, and applying appropriate wound dressings. Keeping the skin clean, moisturized, and monitored is important for preventing complications. Because pressure sores can progress quickly on the lower extremities, especially in people with diabetes or circulation issues, it is suggested that you see a wound care specialist if healing slows down, or symptoms worsen.
Pressure Sores, Pressure Ulcers, and Arterial Ulcers Can Lead to Skin Breakdown
Not all wounds on the feet, ankles, and legs are the same. Pressure sores, pressure ulcers, and arterial ulcers may look similar at first, but develop for different reasons and require specialized care. Understanding these differences is key to proper treatment.
Pressure sores are often caused by friction at common rubbing points. Toes rubbing against each other can create small raw areas, while wearing ill-fitting shoes may lead to sores on the heel, ankle, or sides of the foot. These injuries usually begin at the surface but can quickly deepen if ignored.
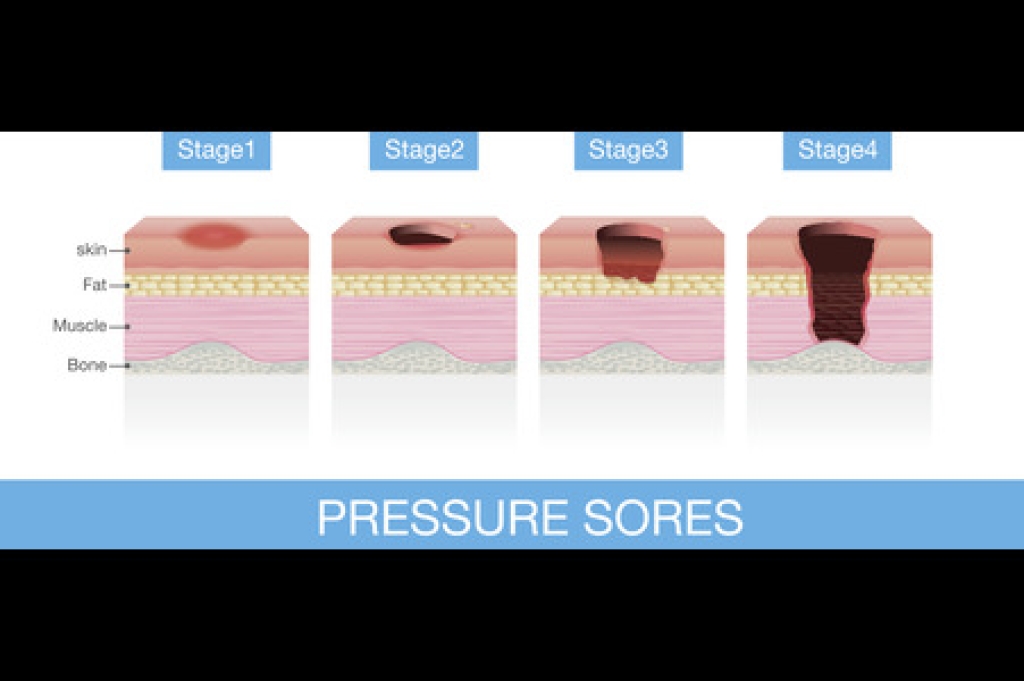
Pressure ulcers, sometimes called bedsores, occur when the skin and tissue are compressed between bone and an external surface for long periods of time. On the lower extremities, they frequently appear on the heels, ankles, calves, or shins. Limited mobility, tight footwear, or prolonged bed rest can all contribute to these ulcers, which may progress through multiple stages from redness to open, infected wounds.
Arterial ulcers are different in that they result from poor circulation. When blood flow to the feet and legs is reduced, oxygen and nutrients cannot reach the tissue. Even small sores on the toes, heels, or shins may become painful, deep ulcers that heal very slowly. Unlike friction-related sores, arterial ulcers are directly tied to vascular health and often signal an underlying circulation problem.
All three types of wounds demand professional attention. A wound care specialist can determine the cause, relieve pressure, improve circulation when possible, and use advanced techniques to promote healing.
If you notice a sore on your foot, ankle, or leg that is slow to close or worsening, call us for timely care to help prevent serious complications and preserve long-term mobility.
